MSU Health Care Gastroenterology Clinic Opens to Serve Greater Lansing
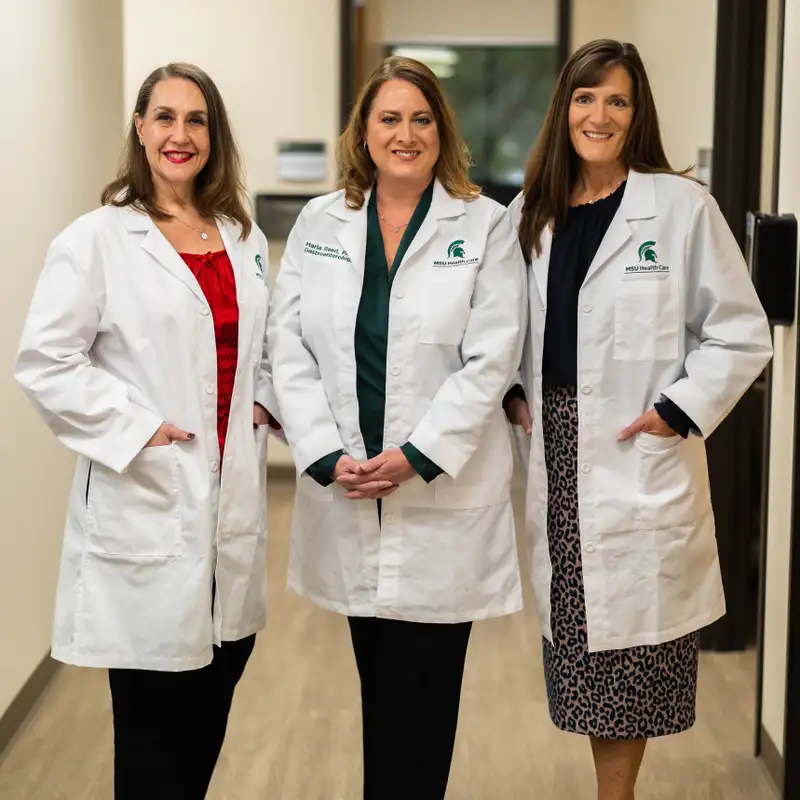
Download MP3After practicing medicine together for over two decades, Dr. Catherine Kerschen, Dr. Lisa Oliveri-LePain and Maria Reed, PA-C, have formed the MSU Health Care Gastroenterology clinic.
“I've been working in gastroenterology for over 20 years,” says Kerschen. “I've been in the mid-Michigan area at different practices. I've actually worked for MSU since 1999. MSU Health Care approached me about starting a practice here at MSU in gastroenterology and we look forward to getting that practice up and running.”
“I've been in practice almost 20 years and I've worked with Cathy and Maria for all of that time in some way, shape, or form,” adds Oliveri-LePain. “I'm a graduate of the MSU College of Osteopathic Medicine, so it's nice to be back where I started.”
“I grew up in the East Lansing and Grand Ledge area, so I know this area well,” Reed says. “I also have worked with Dr. LePain and Dr. Kerschen since 2001. I obtained my undergraduate degree from Michigan State and then went to PA school in Miami, Florida. I'm grateful to be back in the East Lansing area working with these truly great physicians to help satisfy the needs of the East Lansing community.”
So, talk a little bit about why the new practice and you're coming together. What's the goal, the mission?
“The three of us all share the same philosophical goal of wanting a patient-centric community practice where we can take care of the needs of all the people in the Lansing and East Lansing area and some of the outlying areas,” Oliveri-LePain continues. “We’re interested in outreach by helping part of the community that doesn't have the best access to healthcare. Today, nobody should be dying from something like colon cancer. We really want to help the community and build a strong program.”
What is gastroenterology?
“Gastroenterology is the specialty of treating digestive diseases,” Kerschen continues. “We like to say we cover everything from the mouth down to the anus and everything in between. Some of the most common conditions we take care of are colon disorders. Colon cancer screening is something that keeps us busy. We also take care of inflammatory bowel diseases and irritable bowel syndrome. Then we take care of esophageal diseases like acid reflux and peptic ulcer disease. We also cover a variety of liver diseases along with pancreas and gall bladder diseases. We treat a wide range of patients, but we are primarily adult gastroenterologists, so we see patients 18 years and older.”
Who should see you? What symptoms would someone be experiencing to cause them to reach out?
“There are a wide range of symptoms,” says Oliveri-LePain. “You can experience anything from abdominal pain, heartburn symptoms, diarrhea, constipation, and bloating. And sometimes the symptoms are not so obvious, and a lot of symptoms overlap. You can have minor symptoms that can be a symptom of something more serious, something like Crohn's or colitis or something like irritable bowel syndrome where you can have similar symptoms. Treatments are very different though, and they can affect all ages of men and women.”
What is treatment like and what are some of the challenges involved?
“Some of the challenges are environmental like what we eat and the stressors we're under,” Reed says. “We've all been through a lot of stress with COVID, and we try to treat our patients from a holistic approach making sure that they're getting the right nutrition and getting their exercise every day. Medication treatments are also available. We partner with Henry Ford and we're hoping to tap into a lot of research in conjunction with MSU to provide treatments for our patients that might not otherwise be available.”
Is diet the key contributing factor for someone to get a GI disease? Is it hereditary? Why would someone need to see you?
“Every disease entity has a different etiology or risk factors that make it better or worse,” continues Kerschen. “So, in some of our diseases, diet and exercise and mental health make a difference on how well the patient responds. Most colon cancers are sporadic. However, there is an increased risk if you have a family history. So, there can be a genetic link. Some of the liver diseases that we cover have some genetic links, so we'd be more likely to screen patients for certain liver diseases such as hemochromatosis. But a lot of liver diseases are due to risk factors like hepatitis C. If you had a blood transfusion years ago or if you're an IV drug user, that increases your risk. So, we would look at those risk factors for patients. It really depends on what disease we're talking about within the GI system.”
Do patients most often start with their primary care physician and then get referred to you?
“Yes,” says Oliveri-LePain. “The majority of people start out with their primary care physician and then if it gets to a point where they've exhausted their evaluation, they are referred to us. If they need a procedure, they would be referred to us as well.”
Is there some exciting research happening or some new treatments on the horizon that have you excited about treating GI better?
“There are a couple things,” says Kerschen. “In the liver world, there's a lot of research right now on fatty liver, which is a big issue in our society right now. It’s linked with other disease such as cardiovascular disease, diabetes, and obesity. So, liver disease can be linked with that. Right now, all we have is lifestyle changes to help treat it, but there is a lot of research right now going on about different medications that might help with fatty liver. My anticipation would be in the next 10 years that we may have more treatment options for people with fatty liver.
“There's always research going on in a variety of diseases in gastroenterology. Inflammatory bowel disease has something interesting and exciting that they're working on in the research realm. Hopefully again, through our partnership with Henry Ford Hospital, we'll be able to get involved in some of the clinical research.”
Talk about the excitement of coming together and doing what you love to do under the auspices of MSU Health Care.
“To me, this is a perfect union of the three of us because we do know each other so well,” says Oliveri-LePain. “We know how we work philosophically. We are very similar in how we treat our patients. We're going to be able to bring a lot of positive care to the community and to MSU.
“It's important that patients always feel that they're being heard. A lot of patients are tired of the cattle philosophy where they're being herded in and out and they're not really listened to or paid attention to. We think it's important that when patients come in that they're heard and that their concerns are heard and that they're taken seriously. Every patient should know that they're the most important patient at that time. That's really important.”
What would you like our listeners to know about GI diseases and how you can help them?
“One thing that we've seen over the last few years is improvement in our treatment of hepatitis C. Previously when I first started practice, the treatments for hepatitis C were very intense and the success rate was only about 50 percent. Now over the last several years, our treatment success rate is about 96 percent. For patients who may have had hepatitis C for last 30 or 40 years or maybe don't even know they have hepatitis C, the cure rate is phenomenal right now. The treatments are much shorter in duration and the side effects are very minimal. For people who years ago may have had hepatitis C that progressed to cirrhosis and maybe even liver cancer, we don't have that anymore. We would like to be able to have a hepatitis C clinic here in East Lansing at MSU to help those patients.”
“We'd like patients to know that there are a wide variety of GI symptoms that they might be suffering with at home that they don't realize that there's something that can be done about it,” Kerschen says. “I would encourage patients to talk to their primary care physicians because a lot of times there are things that the primary care physician can do for them that will help alleviate it. But when they work with their primary care physician and find that they're still having issues, that's when they'll come to us, and we'll work further to try to figure out what's going on. Particularly in this day of COVID where people aren't asking for help as much for a variety of reasons, we want patients to get back in with their doctors and start talking to them about some of the things that are going on. Then if they need specialists like us, we're now here in the community and we can help work with them and work with their primary care physician to try to improve their symptoms.”
Can you elaborate a little bit more on those symptoms?
“That's a challenging question because depending on what the issue is, you can have minor symptoms like a little bit of belly discomfort or heartburn,” continues Oliveri-LePain. “For people who wake up in the middle of the night with acid issues or a hard time swallowing, it could be something minor like heartburn. Other symptoms are abdominal pain, which can be again from your ribcage all the way down, and diarrhea or constipation. No symptoms should be ignored. So again, start with the primary care physician and then come to us if things don't get resolved.”
“An important part of the gastroenterology practice is that we do endoscopy,” Kerschen adds. “As physicians, we spend a fair amount of time in the endoscopy unit. Right now we'll be working through McLaren Healthcare and Genesis Surgery Center, which is off Jolly Road. That is something that gets arranged through our practice with our schedulers, and we'll take care to make sure our patients are well cared for in those facilities.
“Patients can find us at the Hannah Technical Research Center on Hagadorn. We are on the second floor and our phone number is (517) 353-3102. We share a waiting room with the MSU Urology."
(Photo session followed COVID protocols. Subjects were unmasked briefly.)
MSU Today airs Sunday mornings at 9:00 on WKAR News/Talk and streams at WKAR.org. Find, rate, and subscribe to “MSU Today with Russ White” on Spotify, Apple Podcasts, and wherever you get your shows.
“I've been in practice almost 20 years and I've worked with Cathy and Maria for all of that time in some way, shape, or form,” adds Oliveri-LePain. “I'm a graduate of the MSU College of Osteopathic Medicine, so it's nice to be back where I started.”
“I grew up in the East Lansing and Grand Ledge area, so I know this area well,” Reed says. “I also have worked with Dr. LePain and Dr. Kerschen since 2001. I obtained my undergraduate degree from Michigan State and then went to PA school in Miami, Florida. I'm grateful to be back in the East Lansing area working with these truly great physicians to help satisfy the needs of the East Lansing community.”
So, talk a little bit about why the new practice and you're coming together. What's the goal, the mission?
“The three of us all share the same philosophical goal of wanting a patient-centric community practice where we can take care of the needs of all the people in the Lansing and East Lansing area and some of the outlying areas,” Oliveri-LePain continues. “We’re interested in outreach by helping part of the community that doesn't have the best access to healthcare. Today, nobody should be dying from something like colon cancer. We really want to help the community and build a strong program.”
What is gastroenterology?
“Gastroenterology is the specialty of treating digestive diseases,” Kerschen continues. “We like to say we cover everything from the mouth down to the anus and everything in between. Some of the most common conditions we take care of are colon disorders. Colon cancer screening is something that keeps us busy. We also take care of inflammatory bowel diseases and irritable bowel syndrome. Then we take care of esophageal diseases like acid reflux and peptic ulcer disease. We also cover a variety of liver diseases along with pancreas and gall bladder diseases. We treat a wide range of patients, but we are primarily adult gastroenterologists, so we see patients 18 years and older.”
Who should see you? What symptoms would someone be experiencing to cause them to reach out?
“There are a wide range of symptoms,” says Oliveri-LePain. “You can experience anything from abdominal pain, heartburn symptoms, diarrhea, constipation, and bloating. And sometimes the symptoms are not so obvious, and a lot of symptoms overlap. You can have minor symptoms that can be a symptom of something more serious, something like Crohn's or colitis or something like irritable bowel syndrome where you can have similar symptoms. Treatments are very different though, and they can affect all ages of men and women.”
What is treatment like and what are some of the challenges involved?
“Some of the challenges are environmental like what we eat and the stressors we're under,” Reed says. “We've all been through a lot of stress with COVID, and we try to treat our patients from a holistic approach making sure that they're getting the right nutrition and getting their exercise every day. Medication treatments are also available. We partner with Henry Ford and we're hoping to tap into a lot of research in conjunction with MSU to provide treatments for our patients that might not otherwise be available.”
Is diet the key contributing factor for someone to get a GI disease? Is it hereditary? Why would someone need to see you?
“Every disease entity has a different etiology or risk factors that make it better or worse,” continues Kerschen. “So, in some of our diseases, diet and exercise and mental health make a difference on how well the patient responds. Most colon cancers are sporadic. However, there is an increased risk if you have a family history. So, there can be a genetic link. Some of the liver diseases that we cover have some genetic links, so we'd be more likely to screen patients for certain liver diseases such as hemochromatosis. But a lot of liver diseases are due to risk factors like hepatitis C. If you had a blood transfusion years ago or if you're an IV drug user, that increases your risk. So, we would look at those risk factors for patients. It really depends on what disease we're talking about within the GI system.”
Do patients most often start with their primary care physician and then get referred to you?
“Yes,” says Oliveri-LePain. “The majority of people start out with their primary care physician and then if it gets to a point where they've exhausted their evaluation, they are referred to us. If they need a procedure, they would be referred to us as well.”
Is there some exciting research happening or some new treatments on the horizon that have you excited about treating GI better?
“There are a couple things,” says Kerschen. “In the liver world, there's a lot of research right now on fatty liver, which is a big issue in our society right now. It’s linked with other disease such as cardiovascular disease, diabetes, and obesity. So, liver disease can be linked with that. Right now, all we have is lifestyle changes to help treat it, but there is a lot of research right now going on about different medications that might help with fatty liver. My anticipation would be in the next 10 years that we may have more treatment options for people with fatty liver.
“There's always research going on in a variety of diseases in gastroenterology. Inflammatory bowel disease has something interesting and exciting that they're working on in the research realm. Hopefully again, through our partnership with Henry Ford Hospital, we'll be able to get involved in some of the clinical research.”
Talk about the excitement of coming together and doing what you love to do under the auspices of MSU Health Care.
“To me, this is a perfect union of the three of us because we do know each other so well,” says Oliveri-LePain. “We know how we work philosophically. We are very similar in how we treat our patients. We're going to be able to bring a lot of positive care to the community and to MSU.
“It's important that patients always feel that they're being heard. A lot of patients are tired of the cattle philosophy where they're being herded in and out and they're not really listened to or paid attention to. We think it's important that when patients come in that they're heard and that their concerns are heard and that they're taken seriously. Every patient should know that they're the most important patient at that time. That's really important.”
What would you like our listeners to know about GI diseases and how you can help them?
“One thing that we've seen over the last few years is improvement in our treatment of hepatitis C. Previously when I first started practice, the treatments for hepatitis C were very intense and the success rate was only about 50 percent. Now over the last several years, our treatment success rate is about 96 percent. For patients who may have had hepatitis C for last 30 or 40 years or maybe don't even know they have hepatitis C, the cure rate is phenomenal right now. The treatments are much shorter in duration and the side effects are very minimal. For people who years ago may have had hepatitis C that progressed to cirrhosis and maybe even liver cancer, we don't have that anymore. We would like to be able to have a hepatitis C clinic here in East Lansing at MSU to help those patients.”
“We'd like patients to know that there are a wide variety of GI symptoms that they might be suffering with at home that they don't realize that there's something that can be done about it,” Kerschen says. “I would encourage patients to talk to their primary care physicians because a lot of times there are things that the primary care physician can do for them that will help alleviate it. But when they work with their primary care physician and find that they're still having issues, that's when they'll come to us, and we'll work further to try to figure out what's going on. Particularly in this day of COVID where people aren't asking for help as much for a variety of reasons, we want patients to get back in with their doctors and start talking to them about some of the things that are going on. Then if they need specialists like us, we're now here in the community and we can help work with them and work with their primary care physician to try to improve their symptoms.”
Can you elaborate a little bit more on those symptoms?
“That's a challenging question because depending on what the issue is, you can have minor symptoms like a little bit of belly discomfort or heartburn,” continues Oliveri-LePain. “For people who wake up in the middle of the night with acid issues or a hard time swallowing, it could be something minor like heartburn. Other symptoms are abdominal pain, which can be again from your ribcage all the way down, and diarrhea or constipation. No symptoms should be ignored. So again, start with the primary care physician and then come to us if things don't get resolved.”
“An important part of the gastroenterology practice is that we do endoscopy,” Kerschen adds. “As physicians, we spend a fair amount of time in the endoscopy unit. Right now we'll be working through McLaren Healthcare and Genesis Surgery Center, which is off Jolly Road. That is something that gets arranged through our practice with our schedulers, and we'll take care to make sure our patients are well cared for in those facilities.
“Patients can find us at the Hannah Technical Research Center on Hagadorn. We are on the second floor and our phone number is (517) 353-3102. We share a waiting room with the MSU Urology."
(Photo session followed COVID protocols. Subjects were unmasked briefly.)
MSU Today airs Sunday mornings at 9:00 on WKAR News/Talk and streams at WKAR.org. Find, rate, and subscribe to “MSU Today with Russ White” on Spotify, Apple Podcasts, and wherever you get your shows.
Creators and Guests

Host
Russ White
I host and produce MSU Today for News/Talk 760 @wjrradio and @MichiganStateU's @NPR affiliate @WKAR News/Talk 102.3 FM and AM 870.